
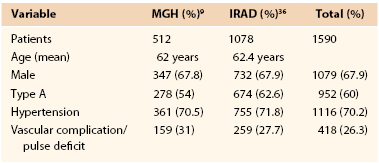
The diagnosis of impending rupture as defined as haemorrhagic pleural effusion or expanding peri-aortic haematoma can only be made with imaging. The role of contrast enhanced imaging cannot be overemphasised as it gives useful information about the predictors of failure, malperfusion, pre-treatment sizing and – most importantly – aortic rupture. Compromised spinal, visceral, renal or iliac blood flow may result in paralysis, paraplegia, lower limb ischaemia, abdominal pain or diarrhoea with raised liver function, amylase, lactate, urea, creatinine and coupled with absence (thrombosis) or delay in contrast enhancement in the target organ. This may be static or dynamic for flow, which can be corroborated by laboratory findings and imaging. 4 End organ dysfunction must be recognised early and is indicative of impending organ failure. Malperfusion may be the presenting feature and occurs in up to 10% of TBAD cases. 7 However, this may only represent the tip of the iceberg because estimates from autopsies suggest that 20–30% cases of TBAD do not make it to hospital. Early high inpatient mortality represents a subset of TBAD due to malperfusion and/or rupture. 5,7 Hypertension is also a predictor for complications, with blood pressure control representing an important goal for management. Hypertension is the second most common presentation according to the International Registry of Aortic Dissection (IRAD) for TBAD, occurring in 66–70.1% of cases. Pain is the presentation in 70–72.4% of cases of TBAD, with people most often experiencing pain in the back or occasionally the abdomen. The classic presentation of TBAD is an abrupt onset of severe sharp tearing or ripping pain in the chest or back. 3,4 TBAD can quickly become catastrophic – in-hospital mortality is as high as 10–14%. It was recognised early on that medical management of type B aortic dissection (TBAD) resulted in good initial results with a review of published literature suggesting a 5-year mortality of 75–88%. Additionally, the timeline from onset of symptoms can divide presentation into acute (3 months). 2 The basis of these classifications was predicated on the vastly different outcomes and treatment modalities for the different presentations.

5 years later in this classification type B signifies that the intimal tear is distal to the left subclavian artery (similar to Debakey type 3). 1 The widely accepted Stanford classification was coined by Daily et al. The first classification of aortic dissection was made by Debakey et al.


 0 kommentar(er)
0 kommentar(er)
